Connect With Us

Foot Stretches for Plantar Fasciitis

Plantar fasciitis causes heel pain due to inflammation of the thick band of tissue along the bottom of the foot. Stretching and strengthening exercises can help relieve discomfort and improve flexibility. A gentle calf stretch, performed by pressing the heel down while leaning against a wall, helps reduce tension in the plantar fascia. Rolling a ball or a frozen water bottle under the foot provides a deep stretch and massage to the arch. Toe stretches, where the toes are gently pulled back toward the shin, can improve mobility and relieve tightness. Additionally, strengthening exercises, such as towel scrunches and toe lifts, help support the foot structure. If you have plantar fasciitis, it is suggested that you consult a podiatrist who can offer effective treatment and relief tips.
Why Stretching Is Important for Your Feet
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Wendy L. Grossman, DPM from New Jersey. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first to determine if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
- Using a foam roller or any cylindrical object (a water bottle or soda can will do), roll the object under your foot back and forth. You should also exert pressure on the object. Be sure to do this to both feet for a minute. Do this exercise three times each.
- Similar to the previous exercise, take a ball, such as a tennis ball, and roll it under your foot while seated and exert pressure on it.
- Grab a resistance band or towel and take a seat. If you are using a towel, fold it length wise. Next put either one between the ball of your foot and heel and pull with both hands on each side towards you. Hold this for 15 seconds and then switch feet. Do this three times for each foot.
- Finally hold your big toe while crossing one leg over the other. Pull the toe towards you and hold for 15 seconds. Once again do this three times per foot.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising to ice and rest the foot. It is advised that you then see a podiatrist for help.
If you have any questions, please feel free to contact our office located in Bloomfield, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stretching Your Feet
Debilitating foot pain is a problem for many people. But just as stretching the torso can help alleviate back pain, stretching the feet can also help mend existing foot problems and prevent future ones.
The feet, as the body’s foundation, carry the body’s entire weight and can get easily strained from overexertion. Persistent sharp pain and cramping in the feet are often common concerns. Foot pain and foot problems can be due to any number of causes, and in many cases pain may be eased without medication or doctor visits. It is always a good idea, however, to first rule out any serious medical issues with a physician.
Stretching can help relax the feet and alleviate pain, but is especially important before heavy aerobic exercise. Stretching before such activities can help you avoid experiencing painful cramps or strained foot muscles. Stretches should be performed slowly and deliberately without forceful pulling. The stretch should be held for several seconds before relaxing.
A great way to stretch out and loosen up the foot muscles while sitting is to cross one leg over the other and pull the toes carefully back without overextending. Start by resting the left ankle on the right knee. With the left hand, gently flex the left foot by pulling back on the toes. Do not pull too hard; just hard enough to feel the stretch in the arch of the foot. Then point the toes of the left foot as far as you can. Rotate the motion of pointing with pulling back on the toes. This should relax and stretch the muscles on the bottom and the top of the foot. Doing this stretch ten to twenty times should bring relief. Repeat the whole process for the other foot by resting the right ankle on the left knee.
A stretch that focuses on the often injured Achilles tendon involves standing and facing a wall with your arms out and hands flat against the wall. Step back with one foot, keeping it flat against the floor. Move the other leg forward and lean toward the wall. You should feel a stretch through the back of your leg and your Achilles tendon, but do not push yourself too much. Stop when you feel a stretching sensation, and hold for 30 seconds. Ten repetitions may be done for each foot.
Stretching the feet is important for athletes or those performing aerobic exercise, but it can also help anyone with foot pain caused by poor footwear, plantar fasciitis, or long hours standing and walking. Individuals who tend to their feet by regularly stretching every day should be able to minimize foot pain and prevent new problems from arising.
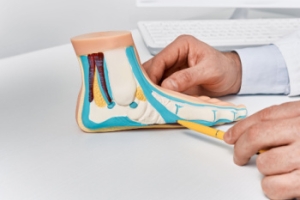
How to Manage the Onset of Flat Feet
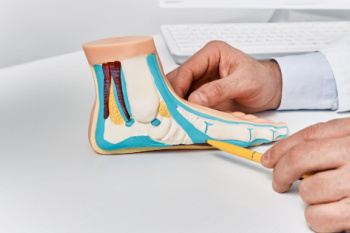
Progressive collapsing foot deformity, also known as adult-acquired flatfoot, occurs when the arch gradually collapses, leading to changes in your foot’s shape and function. Adult-acquired flatfoot often results from dysfunction in the posterior tibial tendon, which plays a key role in supporting the arch and turning the foot inward. As this tendon weakens, the foot may flatten, and the alignment of the ankle can shift, sometimes causing pain or difficulty walking. Aging, previous injuries, obesity, diabetes, or arthritis may contribute to the development of adult-acquired flatfoot. It may result in pain along the inside of the ankle, swelling, or an outward shift of the foot’s position. A podiatrist can assess the severity of the condition using certain imaging tests to determine the best course of treatment. Supportive devices, orthotic inserts, and in more advanced cases, surgery, may help restore function and relieve pain. If you notice that your feet have become flatter, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Wendy L. Grossman, DPM from New Jersey. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Bloomfield, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
Ankle Fracture? Don’t Wait for Treatment
Causes and Prevention of Plantar Warts

Plantar warts are small, rough growths that appear on the soles of the feet, often causing discomfort or pain when walking. They are caused by a viral infection, specifically the human papillomavirus, or HPV, which enters the skin through small cuts or abrasions. The virus thrives in warm, moist environments, making places like public showers, swimming pools areas, and gym locker rooms common areas for infection. To prevent plantar warts, it is essential to avoid walking barefoot in public spaces and to keep feet clean and dry. Wearing moisture-wicking socks and well-fitting shoes can also help minimize the risk. If you have developed a plantar wart, it is suggested that you promptly schedule an appointment with a podiatrist who can provide safe and sterile medical care for relief and removal.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Wendy L. Grossman, DPM from New Jersey. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Bloomfield, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Causes and Prevention of Cuts on Children’s Feet

Children are constantly on the move, making their feet vulnerable to cuts from sharp objects, rough surfaces, or accidental scrapes. These injuries are common in barefoot activities like playing on the beach, running outside, or walking around pools. Cuts can happen to any child, but are more frequent in those who are active or prone to minor accidents. Small cuts are usually cleaned, covered with an antibiotic ointment, and bandaged to prevent dirt and bacteria from entering. Deeper wounds may require butterfly bandages or medical closure strips to keep the skin together while healing. To prevent infection, parents should monitor healing, change dressings regularly, and watch for signs of redness, swelling, or pus. Keeping feet clean and covered in risky environments can reduce injuries. If a cut is deep, slow to heal, or shows signs of infection, it is strongly suggested that you take your child in to see a podiatrist for proper care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Wendy L. Grossman, DPM from New Jersey. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Bloomfield, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Causes of Pain in the Arch of the Feet

Pain in the arch of the foot can greatly impact your daily life, making it challenging to bear weight or walk. This discomfort may result from a variety of conditions, including plantar fasciitis, flat feet, or overpronation. Plantar fasciitis, a common cause, involves inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot. Flat feet, or fallen arches, occur when the arch collapses, leading to pain and strain due to improper distribution of weight. Overpronation, where the foot rolls inward excessively during walking, can also strain the ligaments and muscles, contributing to arch pain. Additional factors such as obesity, ill-fitting footwear, and repetitive high-impact activities can worsen the issue. A podiatrist, a specialist in diagnosing and treating foot conditions, can evaluate your feet to determine the underlying cause of the pain. Treatment may include custom orthotics or specific exercises to relieve pain and improve foot function. If you are experiencing arch pain, it is suggested that you schedule an appointment with a podiatrist for an evaluation and to discuss potential treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Wendy L. Grossman, DPM from New Jersey. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Bloomfield, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.